Lit from within: how tiny wireless bulbs could revolutionise clinical healthcare
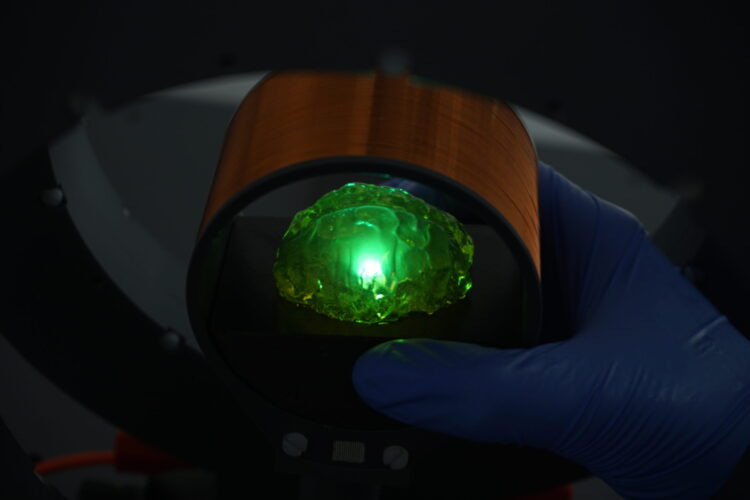
Researchers from the University of St Andrews and the University of Cologne have developed a new device platform that allows for smaller wireless light sources to be placed within the human body.
The new research, published in the journal Science Advances (Wednesday 6 March), indicates that such light sources will enable novel, minimally invasive means of treating and better understanding diseases which currently require the implantation of bulky devices.
Biomedical implants have already revolutionized healthcare, providing life-changing solutions for many individuals. Electrode-based implants, such as cochlear implants, cardiac pacemakers and brain stimulators, function based on the electrical excitability of human cells. They can help to restore hearing, normalize heart function, and mitigate the effects of debilitating diseases like Parkinson’s disease.
The novel approach presented by the scientists from Germany and Scotland is based on the integration of organic light-emitting diodes (OLEDs) on ‘acoustic antennas’. OLEDs are commonly found in modern smartphones and high-end televisions. They consist of thin layers of organic materials which can be deposited on almost any surface.
“We have exploited this property to deposit OLEDs directly on the acoustic antenna, thus merging the unique properties of both platforms into a single, extremely compact device,” explains Professor Malte Gather, from the School of Physics and Astronomy.
The new devices operate at the sub-megahertz frequencies also used in submarine communications, as electromagnetic fields at this frequency are only weakly absorbed by water. However, unlike in submarines, the intended application in biomedicine requires a very small device footprint, so the classical antennas used in our radios and smartphones would be too large at this frequency.
Julian Butscher, who developed the new devices as part of his PhD, said: “Unlike a classical antenna, an acoustic antenna can be very small, even when harvesting energy from a low frequency electromagnetic field.”
The wireless light-emitting device targets optical stimulation that has emerged as a promising alternative to electrical stimulation because it can be more cell selective and even enable the stimulation of individual cells via genetic modification. Such techniques have already shown promising results in early clinical trials, for instance, in treating an otherwise untreatable eye disease.
For many emerging applications, multiple sites must be stimulated independently, which is why modern brain stimulators often incorporate a large number of electrodes. This approach is most prominently pursued by companies like Elon Musk’s Neuralink. The ideal stimulator, however, would consist of tiny, distributed devices, which could be powered and read wirelessly centimetres inside the body, eliminating the need for wires into and through the body altogether.
As is also the case for electrical antennas, and the reason why radio antennas are usually larger than smartphone antennas, the size of both classical and acoustic antennas determines the frequency at which the device operates and in turn the frequency of the magnetic field that is received. This property is exploited by the new wireless light sources: by simply tuning the operation frequency of different acoustic antennas to different values by slightly varying their size, the scientists can operate several of their tiny light bulbs independently, turning each one on and off individually.
In the future, this could allow for the individual addressing of multiple stimulators in different parts of the body, for instance, to treat debilitating neurological disorders.
With their novel device platform, the scientists now move one step closer to developing the ‘ideal stimulator’ by combining minimal device size, low operation frequency, and optical stimulation.
Professor Gather is keen to continue the work: “As a next step, we will work to further reduce the size of our wireless OLEDs and test our technology in an animal model.”
Issued by the University of St Andrews Comunications Office.